The advent of antibiotics turned many once life-threatening diseases into mild ailments. Unfortunately, bacteria reproduce rapidly and easily adapt new gene sequences, making them well-equipped to develop resistance to life-saving drugs, especially when antibiotics are overused or misused.
Infections with antimicrobial-resistant bacteria killed an estimated 1.27 million people worldwide in 2019, according to the World Health Organization (WHO). Here, we take a look at bacteria that the WHO considers critical or high priority. They cause many diseases, especially in low- and middle-income countries where healthcare resources are scarce, and many are able to transfer their genes to other bacteria. This means they can not only avoid antibiotics, but also instruct other microbes how to do so. These are the 10 scariest superbugs in the world.
Related: Dangerous ‘superbugs’ are a growing threat and antibiotics can’t stop their growth. What can?
Carbapenem-resistant Acinetobacter baumannii
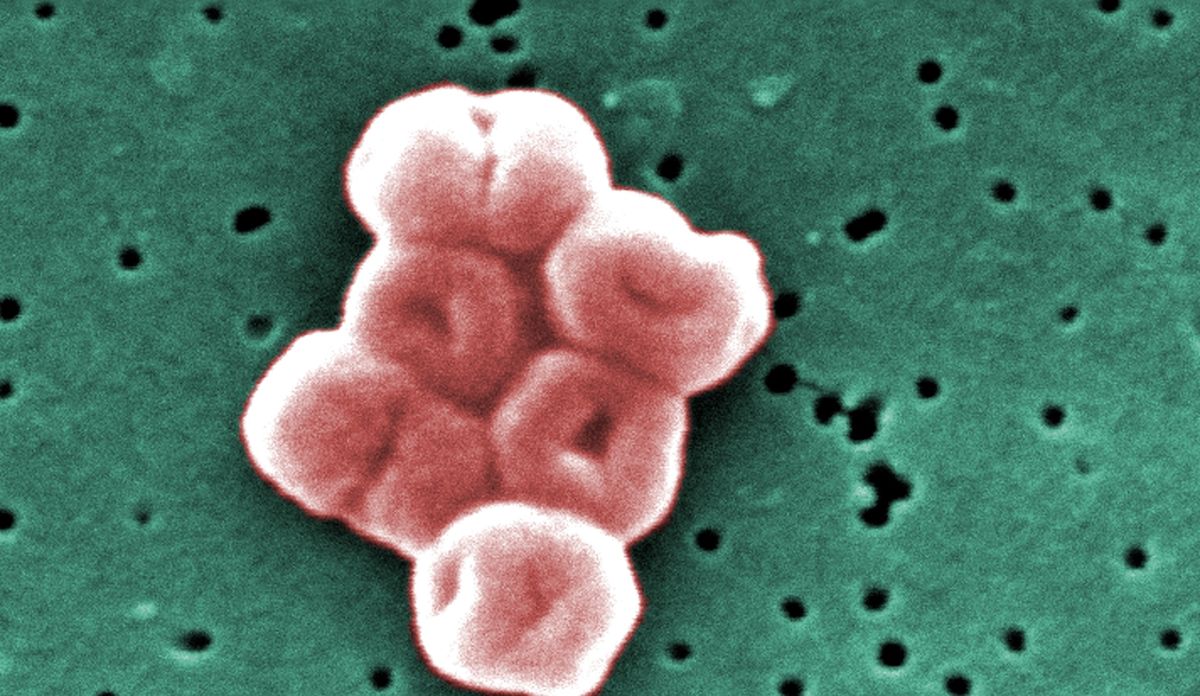
Acinetobacter bacteria are found everywhere, but they are only really dangerous to people in healthcare settings, where most of these infections begin. From this group, Acinetobacter baumannii is the type that most often attacks humans, causing infections in the blood, urinary tract, lungs and wounds, Centers for Disease Control and Prevention (CDC).
The species is opportunistic, infecting people who have weakened immune systems or easy entry routes for the bacteria, such as catheters or surgical wounds. Acinetobacter strains have evolved different types of resistance.
The worst version is carbapenem resistant Acinetobacter baumannii (CRAB). CRAB has genes that produce an enzyme called carbapenemase, which degrades a group of broad-spectrum antibiotics called carbapenems. Worse, according to the CDC, these genes are carried on highly mobile strands of genes called plasmids, which bacteria can easily swap with each other, spreading their resistance abilities. Thus, WHO lists CANCER as a critical public health concern. or 2018 review revealed that the mortality rate from CANCER infections is 47%.
Enterobacteriaceae resistant to cephalosporins and resistant to third-generation carbapenems

Also on the WHO critical list are two types of Enterobacterales bacteria: those resistant to cephalosporins and those resistant to carbapenems. Enterobacterales is an order of bacteria commonly found in the gut; Escherichia coli (E. coli) is one of the most popular, but there are others, such as Klebsiella pneumoniaea common cause of hospital-acquired pneumonia.
Like CANCER infections, Enterobacterial infections are commonly associated with healthcare settings. of CDC estimates that Enterobacterales bacteria caused 13,100 infections and 1,100 deaths in hospital patients in 2017.
Of particular concern are third-generation cephalosporin-resistant Enterobacterales, which are resistant to a group of antimicrobial compounds that used to be a good option for treating resistant bacteria. The loss of third-generation cephalosporins to treat Enterobacterales infections also removes a tool for treating brain infections caused by these microbes, such as antibiotics can cross the blood-brain barrier.
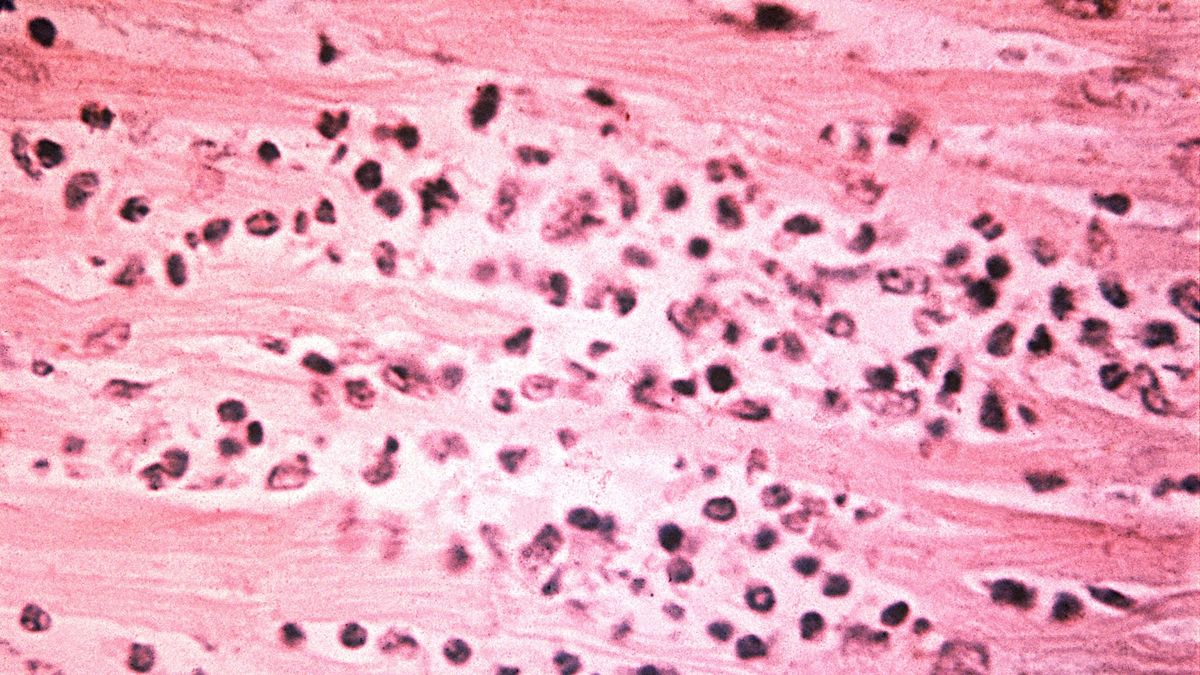
Rifampicin-resistant Mycobacterium tuberculosis

Tuberculosis (TB) is a lung infection caused by bacteria Mycobacterium tuberculosis. Ten million people contract TB each year, according to WHOand over a million die from it every year. These deaths are mostly among the poor in regions where diagnosis and treatment are lacking; Active TB can be cured with six months of treatment with four antimicrobial drugs.
But some types of tuberculosis are resistant to this regimen. Of particular concern, according to the WHO, is rifampicin-resistant TB. According to WHO. Doctors can try different drug combinations for these hard-to-treat cases, but treatment is more complex and often longer than regimens for non-drug-resistant TB. Because of the high burden of disease from rifampicin-resistant tuberculosis, the WHO rates this microbe as a critical concern, urgently seeking new antibiotics to combat it.
Salmonella enterica Typhi resistant to fluoroquinolones
Salmonella enterica Typhus is the bacteria that causes typhoid fever, a serious intestinal infection that causes diarrhea, stomach pain, fever and headache. of WHO estimates that 110,000 people die of typhoid fever every year worldwide. The disease is spread through untreated water and children are at the highest risk of dying from the infection. While typhoid fever is rare in the developed world, it is a major concern in parts of Africa, the Eastern Mediterranean, and parts of Southeast Asia and the Western Pacific, where sanitation and access to medical care are poor.
Typhoid fever used to be easily treated with the antibiotics chloramphenicol, ampicillin, and cotrimoxazole, according to Coalition Against Typhoid. Unfortunately, in the 1970s, a multidrug-resistant strain emerged that could stand up against these first-line antibiotics. In response, doctors turned to fluoroquinolones, another class of antibiotics.
But over the past decade, doctors have increasingly reported disease resistant to treatment with fluoroquinolones. In some regions, typhoid is now treated only by an oral antibiotic, azithromycin, but there are concerns that the superbug is becoming resistant to even this drug. According to the Coalition Against Typhoid, the best strategy is prevention: Hygiene, sanitation and typhoid vaccination can prevent the bacteria from gaining a foothold.
Shigella resistant to fluoroquinolones
Shigella is a genus of bacteria that causes gastrointestinal symptoms, including bloody diarrhea. These infections often clear up on their own, but the disease kills about 200,000 people a year, mostly in lower-income countries with poor sanitation, according to a 2023 paper in the journal. Nature Reviews Microbiology. Young children, the immunocompromised, and the elderly have the highest risk of dying from it Shigella infections.
Treating infection in these at-risk groups has long been possible with antibiotics, but an alarming level of resistance is now emerging, according to the 2023 paper. From their position in the gut, Shigella have the opportunity to mix genes with many other bacterial species, and they have acquired genes to confer antibiotic resistance from these neighbors. Doctors are running out of antibiotic options, the paper’s authors write, and new drugs and vaccines are desperately needed.
Enterococcus faecium resistant to vancomycin
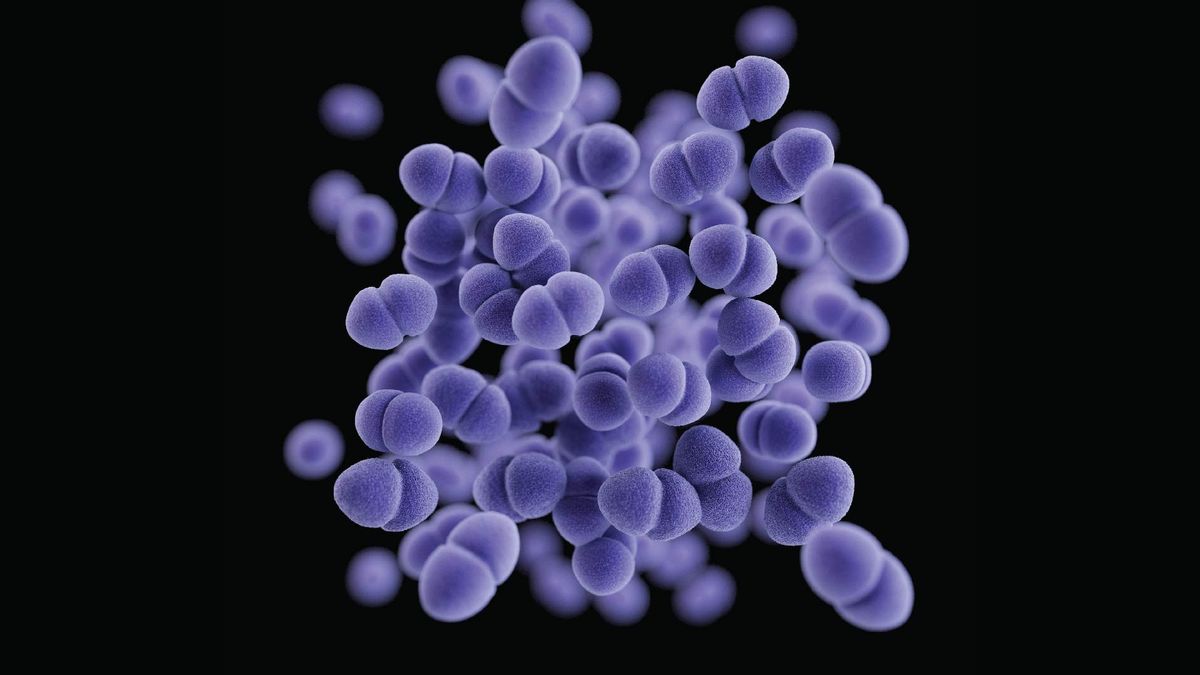
Enterococcus bacteria are usually harmless in the human body, living in places such as the intestines and urinary tract. Sometimes, however, they grow unintentionally or in the wrong place and cause infections. One of the most common friends turned enemy Enterococcus gender is Enterococcus faeciumwhich usually lives in the intestines but can sometimes infect the blood, heart lining or urinary tract, according to a 2018 review.
The antibiotic vancomycin is a necessary drug for these infections, but E. faecium is increasingly resistant. According to New York State Department of Health. As is the case with many common hospital-acquired infections, this microbe preys on older adults and patients with other health conditions.
Carbapenem-resistant Pseudomonas aeruginosa

Pseudomonas aeruginosa it likes moist places like wet soil and can sometimes be found in bathtub drains and on human skin. Even in these cases, the bacteria do not necessarily cause disease. However, especially in patients with coexisting conditionsthe presence of P. aeruginosa portends worse health outcomes. It can also cause life-threatening infections on its own.
WHO lists P. aeruginosa as a serious concern because it is increasingly resistant to carbapenems, antibiotics commonly used to protect against bacteria that have resistance to other first-line antibiotics. This resistance is particularly widespread in South and Central America, according to a 2023 study in The Lancet: Microbe.
Salmonella nontyphoid resistant to fluoroquinolones
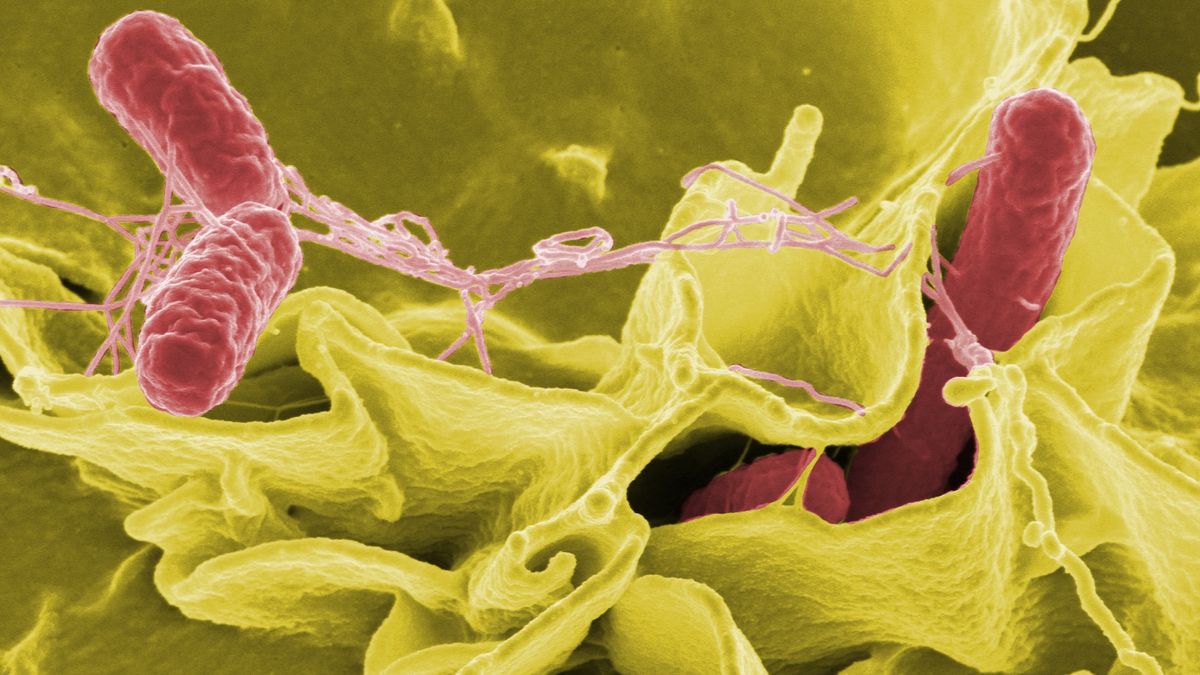
Not all Salmonella strains cause typhus. Many of the 2,500 strains out there result in brief gastrointestinal symptoms, such as diarrhea. This is the type of Salmonella that people sometimes get from undercooked or contaminated food.
Most people will recover from it Salmonella infections without much treatment, and antibiotics are only recommended in cases where the bacteria escapes the gut and spreads to other body systems, according to CDC. But in a growing percentage of these “invasive” cases, doctors are finding that the bacterium is resistant to the first-line treatment, fluoroquinolones. As a backup, doctors sometimes use an antibiotic called ceftriaxone, a cephalosporin. Resistance to ceftriaxone is rare, according to the CDC, but it is increasing in some regions, particularly in sub-Saharan Africa.
Neisseria gonorrhoeae resistant to third-generation cephalosporins and/or fluoroquinolones

Gonorrhea is one of the most common sexually transmitted infections, affecting more than 80 million people annually, according to WHO. If left untreated, it can cause infertility. Antibiotics almost always successfully treat these infections, which are caused by bacteria Neisseria gonorrhoeae.
But over the past few decades, public health experts and doctors have taken notice Increasing antibiotic resistance patterns in cases of gonorrhea. Resistance has been seen around the globe, with a Study 2022 from Bulgaria finding that 59% of cases detected between 2018 and 2021 were resistant to the fluoroquinolone antibiotic. some N. gonorrhea strains are now also resistant to cephalosporins, leaving doctors with fewer tools to fight this common infection.
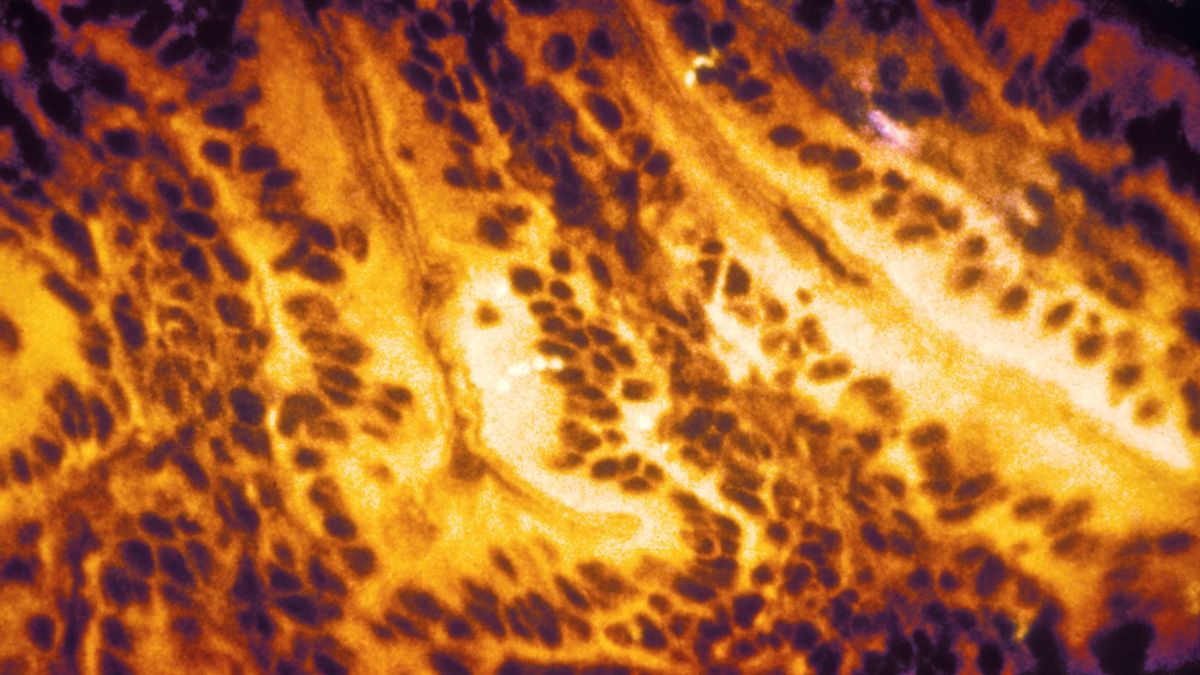
Methicillin-resistant Staphylococcus aureus
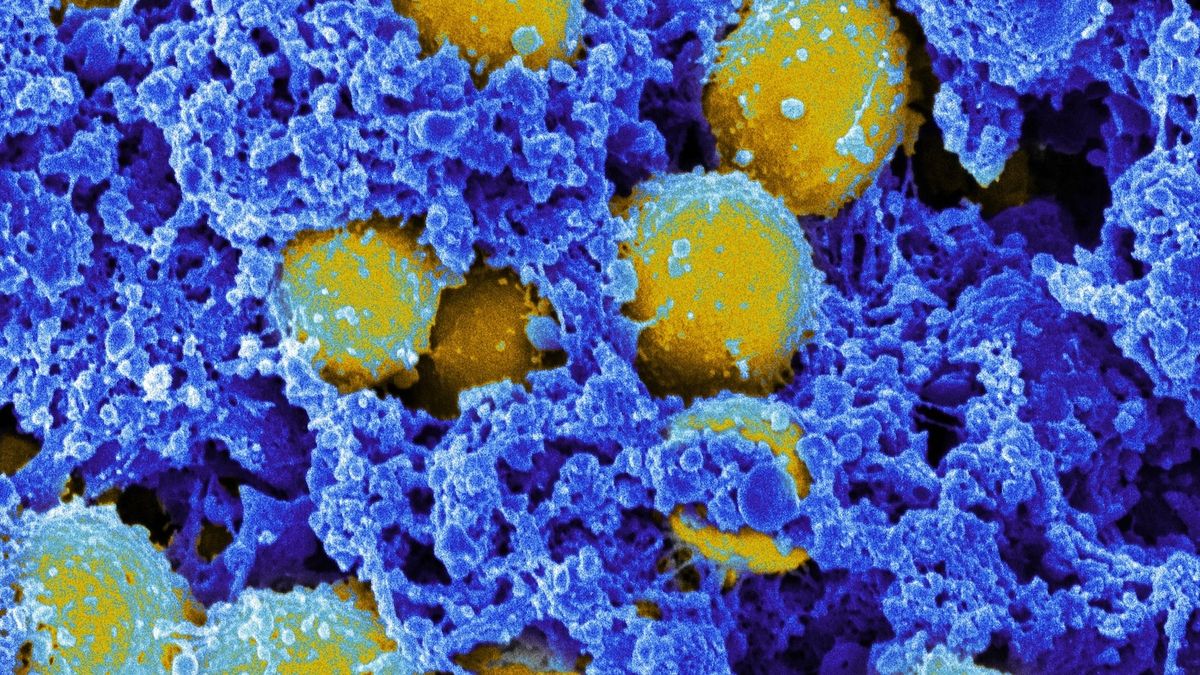
Colloquially known as methicillin-resistant MRSA Staphylococcus aureus is a very common cause of antibiotic-resistant infections. About 1 in 3 people have it S. aureus live harmlessly in their skin. However, if the bacteria grow out of control, the infection can lead to swollen, pus-filled lesions and even progress to an extreme life-threatening immune response called sepsis and even death.
According to CDCsuch as people who live or work in crowded conditions such as military barracks.
As of 2019, MRSA was the single deadliest antibiotic-resistant pathogen globally, according to a study published in the journal. LancetThe resistant form of the germ alone caused more than 100,000 deaths that year alone.
